The World Health Organization (WHO) blueprint for dementia research provides a roadmap to addressing the challenges in the field and reshaping our approach to dementia research. This Comment focuses on how to operationalize the drivers of research highlighted in the blueprint to make research more equitable, impactful and global.
Dementia is one of the greatest health challenges of our generation. With currently 55.2 million people affected worldwide (predicted to reach 78 million by 2030 1 ), dementia is likely to have a critical impact on healthcare systems, care infrastructure and economies. This burden is particularly severe in low- and middle-income countries (LMICs), where currently over 60% of people with dementia live and the largest increase in dementia cases is expected 1 .
International commitments to address the global dementia challenge include the 2013 G8 dementia summit 2 , the adoption of the ‘Global Action Plan on the Public Health Response to Dementia 2017–2025’ (ref. 3 ) and the Okayama Declaration of the G20 Health Ministers in 2019 (ref. 4 ). Yet, dementia research often remains uncoordinated, with disparities in funding and quality 5 . Despite some countries increasing funding for dementia research, overall investment is not proportionate to the impact and cost of dementia 5 .
Accelerating research efforts is crucial for addressing any global health challenge. The COVID-19 pandemic has shown how quickly research can advance when the international community works together. However, it has also highlighted the unequal access to biomedical advances and research infrastructure globally, as well as the need to shift our approach to research toward global public-health interests.
Notwithstanding the challenges, our knowledge about dementia has substantially increased over the past four decades and many scientific advances — although mostly seen in high-income countries (HICs) — have improved diagnosis and care for people with dementia 6 . However, there is still no cure for dementia and most countries are not acting on dementia risk reduction, despite the growing evidence in its support. A holistic approach to science is needed that focuses on all aspects of research, including basic and clinical research, and its implementation into practice and policy.
To this end, the WHO has developed a blueprint for dementia research 7 , the first WHO blueprint to focus on a noninfectious disease. The blueprint aims to support the global prioritization of dementia research and provides a coordination mechanism to facilitate timely and high-quality evidence generation, fast-track innovation, foster effective research implementation and guide resource mobilization.
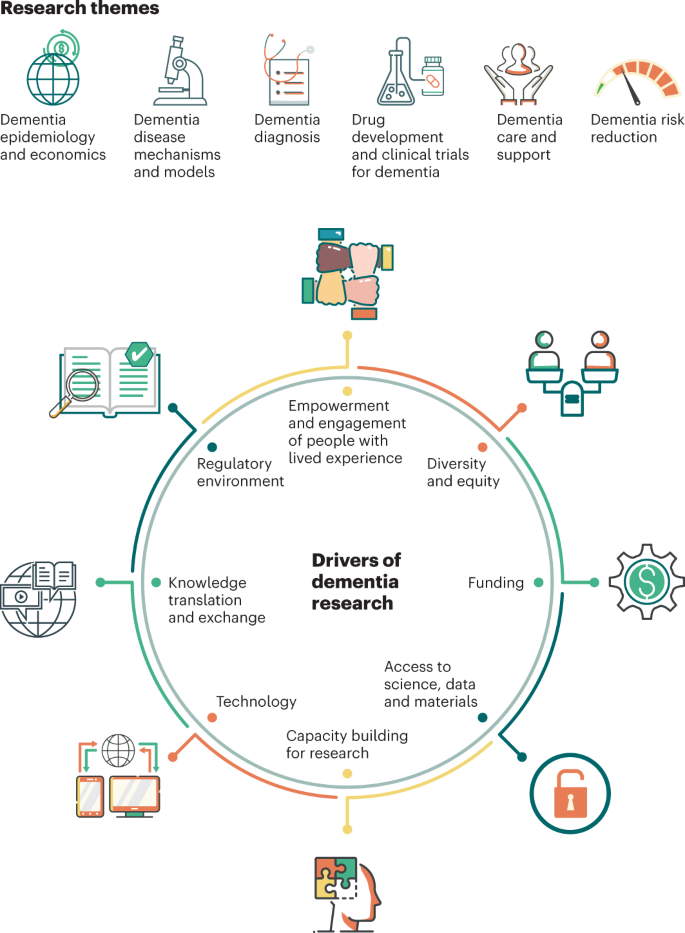
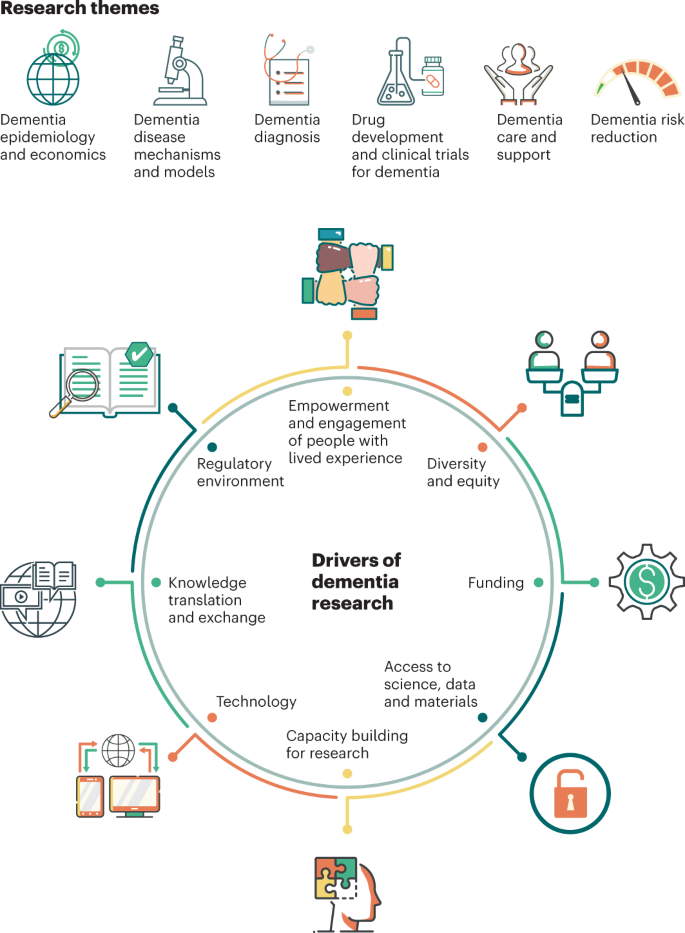
The blueprint summarizes the current state of dementia research across six research themes (Fig. 1), highlights gaps, and outlines strategic goals and actions to address them. Addressing the gaps requires an enabling research environment that can be achieved through eight essential drivers of dementia research (Fig. 1) that together ensure greater efficiency, equity and impact. This Comment focuses on how these drivers of research can be operationalized by different stakeholders to foster long-term systemic changes that strengthen dementia research globally.
Globally, people with dementia are insufficiently involved in all stages of research, ranging from priority setting, planning and development of research proposals to knowledge translation and integration in policy. Data from WHO’s Global Dementia Observatory show that in almost 50% of countries, people with dementia are not at all involved in research 1 .
The blueprint therefore calls for the mandatory inclusion and active involvement of people with dementia and their carers. Concretely, the research community in partnership with civil society should develop, for example, programs that provide training in research and science so that people can contribute in a meaningful way and create processes that account for different levels of cognitive, sensory and physical impairment or disability.
Traditionally, dementia research has been driven by and conducted in HICs. For instance, genetic data are mainly representative of populations of European origin 7 . Inequities also exist in terms of funding allocation, which negatively affects mostly women and researchers from LMICs 1 . The blueprint therefore outlines equity principles to be applied by funding bodies, regulatory authorities and the scientific community (such as fairness and equal participation in resource allocation and in representation in studies) that foster real, transparent research collaborations, decrease the power imbalance and dependence on HIC institutions, as well as increase research output and the representation of LMICs in global dementia research. Funding bodies, for example, can increase the diversity of funding streams to reflect all priority areas and actively seek submissions that address inequities and promote equal partnerships between HICs and LMICs.
To promote diversity and inclusion of populations and communities who are traditionally less likely to participate in dementia research or are rarely covered by scientific studies (for example, epidemiological research), funders and research institutions can develop equity monitoring systems to ensure better representativeness and a fair distribution of resources.
Dementia research has been chronically underfunded and unevenly distributed. Of the 50 organizations and institutions that received the most grants for dementia research in 2019, 41 were in the USA, 6 in the UK and 3 in Canada 8 . This discrepancy also results in research collaborations being predominantly established with other HIC institutions 8 .
To address this imbalance, funding agencies can strategically allocate resources to LMICs towards building research capacity and infrastructure, and support the perennial development and training of a research workforce. The extent to which funders implement such recommendations can be monitored by measuring the proportion of awards being allocated to collaborations between HICs and LMICs in the design and execution of studies, as well as to researchers with geographical, gender and background underrepresentation.
The duration and continuity of funding are also crucial. Given the chronic and often slowly progressive nature of dementia, continuous funding must be provided for comprehensive longitudinal research, which is often costly. This can be facilitated by increased advocacy for resource allocation to dementia research, as well as the establishment of collaborations between funders to jointly develop funding calls. Funding agencies should strive to achieve a better balance by including underresearched aspects of dementia, such as conditions other than Alzheimer’s disease or dementia in highly vulnerable or marginalized populations.
Access to scientific knowledge, data and materials is limited in many parts of the world, with international restrictions interfering with the ability to share biosamples. Simultaneously, a lack of international standards, regulations and incentives can also hinder the ability to share materials and data. Moreover, insufficient researcher time, lack of funding, inadequate storage infrastructure and the fact that funders do not fully mandate open access to data 9 further hamper routine data sharing and global access to science.
To facilitate scientific data sharing and collaboration, governments can review existing laws and regulations concerning data sharing and protection or develop new ones, and funding agencies can promote the responsible and ethical use of data by mandating data sharing or providing incentives to do so within existing regulations.
Access to science has often been pay-walled by publishers, which creates barriers — especially in low-income settings. Recent efforts to make scientific literature more accessible through open-access publishing are encouraging, and the exemption from payment of open-access publishing fees to scientists from low-resource countries can substantially help to develop and foster scientific enterprise in LMICs.
Research career pathways are often insecure in dementia, owing to scarce funding and support. As a result, promising researchers (particularly women and junior researchers) may seek alternative careers, which cause a ‘brain drain’ and a reduction in research capacity 10 .
To address this, the blueprint calls for long-term strategies to invest in and build research capacity across all income settings. For instance, the academic sector should provide researchers in disciplines that are relevant to dementia research and related areas (such as aging, noncommunicable diseases and mental health) with training and resources in basic science, epidemiology, cognitive assessment, ethical research practice and dementia care, particularly in areas and settings where skills are lacking. This will strengthen capacity and broaden the pool of scientists working on dementia, and lead to a greater impact in areas such as epidemiology, disease mechanisms and risk reduction.
The career paths of female researchers also require increased attention, with academic institutions fostering their development and ensuring a fair representation in professorship and management positions. Likewise, junior researchers experience uncertainties regarding their career development. Addressing this issue requires the relevant government sectors to jointly develop strategies to provide more tenure-track positions, instead of short-term development grants and temporary positions.
Often considered a new determinant of health 11 , digital technologies have tremendous potential to improve the quality and reach of healthcare. Wearable devices and smartphones, for example, can collect large amounts of continuous real-time data that can be integrated and harmonized by big-data technology at different scales. However, 37% of the world’s population is still offline 12 , hampering the access to potential health benefits for many populations.
To achieve substantial global progress and eliminate the ‘digital divide’ both within and between HICs and LMICs, and across gender and socioeconomic lines, governments, funders and the private sector must invest in technological health infrastructure where it is currently lacking and ensure that innovations are applied and scaled to the benefit of societies and the elimination of health inequity. Similarly, legal frameworks regulating the access, use and protection of personal data need to be developed and regularly reviewed.
Across all income settings, infrastructure should be developed, and training provided to apply approaches grounded in data and enable the application of artificial intelligence such as machine-learning and deep-learning to dementia research. Open-source and offline software should be developed through public–private partnerships to support digitally disadvantaged groups, while an increase in capacity and investment takes place.
The time gap between evidence generation and its implementation in clinical practice is often too long 13 . Similarly, the translation and uptake of evidence into policy is also hampered owing to lack of awareness from policy-makers and communication between the various sectors 7 .
The blueprint therefore emphasizes the need for increased efforts and dedicated resources to disseminate research evidence to relevant stakeholders in a timely manner. It is also key to specifically strengthen the field of implementation science through long-term strategic investment and requirements for grant proposals to include implementation strategies, either into policy or practice, when relevant.
Often, knowledge, skills and infrastructure that are required for dementia research and implementation may not be present in all settings. To address this, the research community can share expertise by building strong international networks, shared databases and platforms that link diverse researchers, facilitate multidisciplinary collaboration and ensure that research findings can be implemented in diverse settings at local, national and international levels.
Regulatory frameworks for drug development and clinical trials are sometimes seen as barriers to research progress. However, a strong, well-formulated and transparent regulatory environment is a key driver of research and an important enabler of collaboration and successful research implementation. Complexity and a lack of transparency in regulatory environments, combined with divergent international norms and standards, may create barriers that will hinder the establishment of collaborations and slow down the implementation of innovations 7 .
This warrants the creation of ethically sound guidelines by regulatory agencies that anticipate the evidence and requirements necessary for regulatory review and policy development, to fast-track life-changing scientific advances. This would be further facilitated by international harmonization of norms and standards and international agreements for the establishment of worldwide collaborations.
All stakeholders have a role in operationalizing these interconnected drivers of dementia research and making research an integral part of the public health response to dementia, fully recognizing the wide societal impact of dementia with consequences that span well beyond the healthcare and social care sectors.
As outlined here, national and international research agencies and funding bodies should use this blueprint to inform their funding streams and research efforts. Civil society can support advocacy efforts that align with this blueprint, aiming to create a more equitable, efficient and collaborative research landscape. Researchers can also contribute by addressing the identified research gaps. Adopting this comprehensive approach will contribute positively to the promotion and protection of overall brain health. The WHO will use its convening power to bring together stakeholders, including regulatory bodies, funders and the scientific community, to advance the actions outlined in the blueprint.
The WHO gratefully acknowledges the financial support of Gates Ventures for the development of the WHO blueprint for dementia research. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.